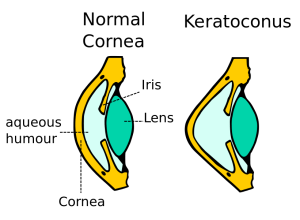
Keratoconus is an eye condition that develops when the tissue within the cornea thins and weakens. It causes the cornea to bulge into a cone-like or rugby ball shape. This condition affects approximately 1 in 500 people. Those affected with keratoconus typically start experiencing symptoms as teenagers or young adults, and it may progress slowly over time. Many people have mild keratoconus (and are unaware) and believe it is just astigmatism. But their vision is corrected with glasses or toric lenses. and it does not affect their daily life.

There are many different causes of keratoconus. For some people, it runs in their family. For others, it can be due to a history of excessive eye rubbing from eye allergies and various other medical conditions. Sometimes it can be secondary to laser vision correction performed on a patient not properly screened. It has a higher prevalence in certain communities, teenage boys and those with Ehlers Danlos Syndrome, pregnant women, and Downs Syndrome.
Symptoms of keratoconus
Keratoconus causes vision to slowly worsen over time and is usually asymmetric (one eye affected more than the other). While it does not cause blindness, it makes people more dependent upon glasses and contact lenses. In advanced cases, vision can only be corrected with hard contact lenses or surgery.
Primary symptoms include:
- Gradually decreasing vision in one or both eyes
- Double vision when looking with just one eye
- Objects both near and far look distorted and blurred, even when wearing corrective glasses or contacts
- Halo and glare around lights in high contrast situations, like streetlights, when driving at night

How is keratoconus diagnosed?
If you are experiencing changes in vision as described above, you should book an appointment to see an eye doctor, or optometrist. Your doctor will check your prescription and examine your eyes.
If the cornea shows signs of bulging, which is typical of keratoconus, your doctor may use several different instruments to measure the curvature of the eye. The primary method involves using a topographer, which measures the shape and thickness of your cornea to create a three-dimensional “map” of your cornea. This process is painless, quick and does not touch the eye.
Early detection is important for monitoring purposes. If any progression is detected, treatment can reduce further vision loss. Additionally, if you have any risk of keratoconus, it is important not to proceed with laser vision correction surgery such as LASIK or SMILE, which can worsen the condition. A condition known as corneal ecstasia is a common side effect of LASIK surgery, which presents the same as keratoconus and is treated in the same way.
How is keratoconus treated?
Treatment usually starts with new eyeglasses. New eyeglasses can usually make vision clear again in mild cases of keratoconus. Eventually, though, it may be necessary to use contact lenses.
In cases where keratoconus progresses over time, corneal cross-linking is performed to strengthen the cornea, stop the thinning process, and stabilize the cornea. This procedure can stop further vision loss, and in some cases, vision can gradually improve over time. CXL can be done more than once, and also on a grafted cornea to strengthen it in specific areas i.e. the edges.

What is corneal cross-linking?
Normal corneas have cross-links between the collagen fibers that keep them strong and able to retain their normal shape. With keratoconus and related disorders, the cornea is weak with too few cross-links or support beams. This weakening allows the cornea to bulge outwards.
The cross-linking procedure adds cross-links or “cross beams” to the cornea. This makes the cornea more stable and helps it hold its shape and focus better.
What other treatments are available for keratoconus?
Specialty contact lens fitting involves fitting keratoconus corneas with bespoke contact lenses. These are widely available on the NHS and in private clinics.
EVO implantable Collamer lens placement is sometimes performed on stable adult keratoconus patients who can see well with eyeglasses. In this procedure, an intraocular lens is placed inside the eye to correct the prescription and eliminate the need for glasses or contact lenses.
Corneal transplant/graft – see our comprehensive guide here, this surgery is always the last option when no lenses can be worn
Learn more –

Leave a comment